 Each February the World Health Organization (WHO) convenes a panel of epidemiologists and virologist to review influenza serotypes isolated and characterized by the Global Influenza Surveillance and Response System from patients in the Southern hemisphere. Based on the results from as many as 120 collaborating influenza reference centers, the panel selects from among influenza A and influenza B strains to be included in the annual influenza vaccine. For the 2021 -2022 season the strains in the U.S. vaccine are:-
Each February the World Health Organization (WHO) convenes a panel of epidemiologists and virologist to review influenza serotypes isolated and characterized by the Global Influenza Surveillance and Response System from patients in the Southern hemisphere. Based on the results from as many as 120 collaborating influenza reference centers, the panel selects from among influenza A and influenza B strains to be included in the annual influenza vaccine. For the 2021 -2022 season the strains in the U.S. vaccine are:-
- A/Victoria H1N1
- A/Cambodia H3N2
- B Washington 2019-like Victoria lineage virus
- B Phuket 2013-like virus
The selection of strains to be included in the annual vaccination is based on value judgment and risk assessment but the decision of the panel is not infallible. The emergence and spread of influenza viruses during the upcoming 2021-2022 influenza season in the northern hemisphere may diverge from the pattern of previous years. The incorporation of influenza A and B strains may not be appropriate to the challenges that emerge. The precautions adopted in 2020 to prevent dissemination of SARS-CoV-2 responsible for COVID including masking, social distancing and home confinement limited the spread of influenza during the 2020-2021 season. Accordingly the WHO panel was limited in their decision on selection of strains. A second problem relates to the fact that in the absence of influenza challenge, a high proportion of the population in the Northern hemisphere nations will have greater susceptibility to strains of the virus that may emerge.
 Using egg-propagation with appropriate quality control and the restraints relating to distribution, the vaccine combination as selected by the panel is released each year in October and is now available for administration in the U.S.
Using egg-propagation with appropriate quality control and the restraints relating to distribution, the vaccine combination as selected by the panel is released each year in October and is now available for administration in the U.S.
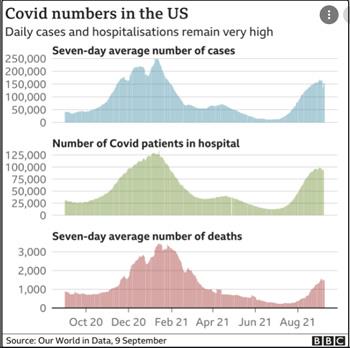
Epidemiologic research has demonstrated that the severity of influenza as measured by incidence rate and mortality is greater in years following a mild influenza season. Every effort must therefore be made to immunize our population especially those working in confined spaces including egg packing plants, and facilities processing red meat and poultry. Unfortunately COVID is still a problem despite a slight decrease in incidence rate attributed to vaccination and public health measures. Notwithstanding progress in vaccine acceptance, 40 percent of our population is vulnerable to COVID many of whom are clustered in rural areas of southeastern and northwest states. Co-infection with both influenza and SARS-CoV-2 does occur and would be expected to result in more severe clinical effects than either disease alone. A winter surge in influenza complicated by COVID will create problems for diagnosticians especially if respiratory syncytial virus complicates an ongoing “twinfection” of COVID and influenza. This will especially be the case for children since availability of an mRNA vaccine at an approved dose will probably not be available before late November.
 In anticipation of a season characterized by severe respiratory complication from viral infections, a higher proportion of our population must be vaccinated against both COVID and influenza.
In anticipation of a season characterized by severe respiratory complication from viral infections, a higher proportion of our population must be vaccinated against both COVID and influenza.
More antigen testing kits with high specificity will be required to enable physicians to rapidly distinguish among the three important respiratory viral infections in order that appropriate medication can be initiated. Antiviral therapy is now available for both influenza and COVID, albeit at high cost for the latter disease. Experience has shown that prevention through vaccination is far more effective and less expensive than treatment. This justifies campaigns to increase immunity among plant and farm workers and their families and the communities in which they live.
In years to come, we may have available mRNA vaccines against multiple strains of influenza and even against combinations of influenza and COVID. In the interim we will have to rely on the traditional approach involving selection of most probable strains of influenza and the time restraints associated with either egg or tissue-culture propagation.
The bottom-line message is for public health authorities and employers to encourage vaccination against both COVID and influenza in advance of what may be a season characterized by severe respiratory disease with the potential for hospitalization and mortality.